Fever and Temperature Taking
Fever and Temperature Taking
Babies younger than 6 months old should see a doctor when they have a fever. Do not use a mercury thermometer. If it breaks, you might be exposed to this toxic substance.
Medication is not always needed to reduce a child’s temperature. When your child is sick with an infection (bacterial or viral), it is common to also have a fever. Fever will not hurt your child. Usually, it goes away after 72 hours (3 days).
Babies younger than 6 months old should see a doctor when they have a fever. Older children can be treated at home, as long as they get enough liquids and seem well otherwise. However, they should see a doctor if their fever lasts for more than 72 hours.
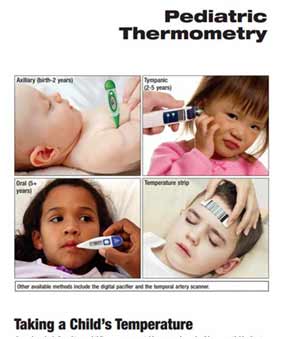
There are several ways to take your child’s temperature:
- rectal method (by the rectum or ‘bum’)
- oral method (by the mouth)
- axillary method (under the armpit)
- temporal artery method (forehead)
- tympanic method (in the ear)
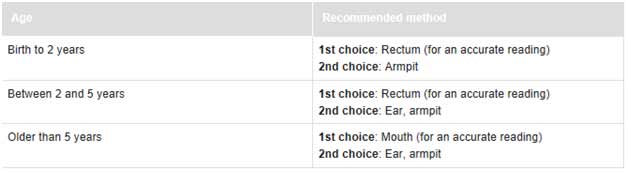
Which method should I use?
The right method depends on your child’s age. It’s important that the measurement is accurate. Use this chart to help you decide which method to use.
Temperature-taking tips
- Do not use a mercury thermometer. If it breaks, you might be exposed to this toxic substance.
- Do not use an oral thermometer to take a rectal temperature, or a rectal thermometer for oral temperature taking.
- A digital thermometer can be used for both rectal and oral temperature taking. It’s made of unbreakable plastic, is easy to read and measures temperature quickly.
- Products for taking temporal artery temperature (sweeping thermometer across your child’s forehead) at home are not accurate or reliable enough.
- Fever strips are not recommended because they do not give accurate readings.
To get an accurate reading of your child’s temperature, you’ll need to make sure it’s done right.
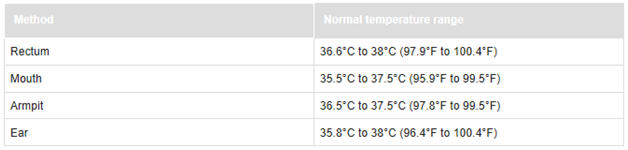
What is a normal temperature?
The following chart will tell you if your child has a fever. The normal temperature range varies and depends on the way you took your child’s temperature.
The degree (height) of a fever does not tell you how serious your child’s illness is—how your child is acting is usually a better sign. A child with a mild infection can have a high fever, while a child with a severe infection might have no fever at all.
What can I do if my child has a fever?
Keep your child comfortable, and offer plenty of fluids. If your baby has a fever, remove extra blankets and clothing so heat can leave her body and help lower the body temperature. But don’t take off all your child’s clothes, because she may become too cold and start shivering, which makes more body heat and will cause her temperature to rise again.
Sponging your child with lukewarm water, alcohol baths and rubs is not recommended.
Medication is not always needed to reduce a child’s temperature. In fact, the best reason for giving your child medicine is not to reduce the fever, but to relieve any aches and pains.
Acetaminophen (such as Tylenol, Tempra, Panadol and others) is a suitable medication for a fever. Unless your doctor says otherwise, you can give the dose recommended on the package every 4 hours until your child’s temperature comes down. The temperature usually comes down in 1 hour and then rises again. If this happens, the medication may have to be repeated at the recommended time. Do not give more than 5 doses in 24 hours.
Alternatively, you can give your child ibuprofen, which is found in products such as Advil and Motrin. Be sure to follow the directions on the package. Ibuprofen can be given every 6 to 8 hours — up to 4 times in a 24-hour period. Do not exceed the recommended dose.
- Ibuprofen should only be given if your child is drinking reasonably well.
- Do not give ibuprofen to babies under 6 months without first talking to your doctor.
Do not alternate between using acetaminophen and ibuprofen as this can lead to dosing errors.
A child or teenager with a fever should not be given aspirin [acetylsalicylic acid (ASA)]. If the fever is due to chickenpox, influenza or certain other viral infections, taking aspirin can increase the risk of Reye’s syndrome. This is a very serious condition that can damage the liver and brain.
Contact your health care provider if your child:
- Has a fever and is less than 6 months old.
- Has a fever for more than 72 hours.
- Is excessively cranky, fussy or irritable.
- Is excessively sleepy, lethargic or does not respond.
- Is persistently wheezing or coughing.
- Has a fever combined with a rash or any other signs of illness that worry you.
This is the most reliable way to ensure a fever is not missed.
- Clean the thermometer with cool, soapy water and rinse.
- Cover the silver tip with petroleum jelly (such as Vaseline).
- Place your baby on his back with his knees bent.
- Gently insert the thermometer in the rectum, about 2.5 cm (1 inch), holding it in place with your fingers.
- After about 1 minute, you will hear the beep.
- Remove the thermometer and read the temperature.
- Clean the thermometer.
The oral method is not recommended for children younger than 5 years old because it is hard for them to hold the thermometer under their tongue for long enough.
- Clean the thermometer with cool, soapy water and rinse.
- Carefully place the tip of the thermometer under your child’s tongue.
- With your child’s mouth closed, leave the thermometer in place for about 1 minute, until you hear the beep.
- Remove the thermometer and read the temperature.
- Clean the thermometer.
The armpit (axillary) method is usually used to check for fever in newborns and young children, but it’s not as accurate as a rectal temperature. If an axillary temperature does not show a fever but your child feels warm and seems unwell, take a rectal measurement.
- Use a rectal or oral thermometer.
- Clean the thermometer with cool, soapy water and rinse.
- Place the tip of the thermometer in the center of your child’s armpit.
- Make sure your child’s arm is tucked snugly against her body.
- Leave the thermometer in place for about 1 minute, until you hear the “beep.”
- Remove the thermometer and read the temperature.
- Clean the thermometer.
Though quick to use, the ear (tympanic) method can give temperature readings that are too low, even when the manufacturer’s directions are followed. It is not as reliable or accurate as rectal temperature taking.
- Use a clean probe tip each time, and follow the manufacturer’s instructions carefully.
- Gently tug on the ear, pulling it back. This will help straighten the ear canal, and make a clear path inside the ear to the ear drum.
- Gently insert the thermometer until the ear canal is fully sealed off.
- Squeeze and hold down the button for one second.
- Remove the thermometer and read the temperature.
Febrile seizures
Febrile seizures
What are Febrile Seizures?
Febrile seizures are convulsions caused by fever. They happen in 2 to 5% of children between the ages of 6 months and 5 years The older your child is when he has his first febrile seizure, the less likely he will be to have more. If a family member (sibling, parent, aunt or uncle, grandparent) has febrile seizures, your child may be more prone to them.
- How will I know if my child is having a febrile seizure?
- What can parents do?
- When should I call the doctor?
Often the seizure is the first sign of your baby’s fever. It can be scary to see but they aren’t as dangerous as they look.
- Your child will have a fever higher than 38⁰C (100.4⁰F)
- Her body will stiffen.
- Her eyes will roll upward and her head and limbs (arms, legs) will be jerky.
- She may briefly lose consciousness.
Most febrile seizures last between 30 seconds and 2 minutes and don’t have any long term effects.
- Stay calm.
- Place your child on a flat surface on his side. Do not move him unless he is near something dangerous. Do not restrain him (hold him down).
- Wipe away any vomit or saliva outside his mouth, but do not put anything between his teeth.
- After the seizure stops, keep your child on his side.
- Allow him to sleep after the seizure and wake him up gradually.
- Call an ambulance or rush to nearby emergency room if the seizure lasts longer than 3 minutes or if your baby is younger than 6 months.
- Visit your doctor for a physical exam to rule out any other problems within a few hours of any seizure, even a brief one.
Healthy Bowel Habits for Children
Healthy Bowel Habits for Children
The most common problems with bowel movements are constipation and diarrhea. Do not rush toilet learning. Children can worry and hold back bowel movements if they feel pressured. Try to get your child used to a regular daily toilet routine. There are many causes of diarrhea, though it’s usually caused by a virus.
Regular bowel movements are important to your child’s health. Bowel habits—how often, how much, and so on—will vary from child to child. Some children go more than once a day, while others may skip a day or two. You can encourage healthy bowel habits by:
- Eating healthy foods — whole grains, fruits and vegetables — and drinking more water each day. Children should have no more than 120 ml of 100% fruit juice per day.
- Staying active throughout the day. This will help keep bowels working well.
- Teaching your child not to hold a bowel movement.
- Explaining that regular bowel movements are normal and important for good health.
- Not using negative words like “dirty” or “stinky,” because they can make your child feel self-conscious about going to the toilet.
The most common problems with bowel movements are constipation and diarrhea.
When should I call my doctor?
Call your doctor if your child:
- Has diarrhea and is younger than 6 months of age.
- is often constipated.
- has bloody or black stool.
- is toilet trained, but starts to lose some control of her bowel and has accidents in her underwear.
- has diarrhea and a fever with a temperature higher than 38.5°C (101.5°F).
- has signs of dehydration (increased thirst, no tears, peeing less, dry skin, mouth and tongue, faster heartbeat).
- Is not gaining weight.
What are symptoms of constipation?
Constipation can happen when bowel movements:
- are passed less often than usual, and/or,
- hard and dry, and difficult or painful to pass, and/or
- stool seems unusually large for your child.
Constipation can cause stomach pain and bright red blood on the surface of a hard stool.
If your child is constipated, it may seem like he is straining to go to the bathroom. In fact, he is holding it in because it hurts to go.
What causes constipation?
- A low-fibre diet that doesn’t include enough whole grains, fruits and vegetables. Products with more than 4 grams of fibre per serving (listed on the package) are good sources of fibre.
- Too much milk, juice, or other dairy products can cause your child to feel full. That means she’ll eat less of other foods that help her bowels work well.
- Being afraid to use the toilet. Your child may also hold back a bowel movement if there is a crack or tear around the anus, causing pain.
- Not enough physical activity.
- Some kinds of medicine can cause constipation.
What can I do if my child is constipated?
- Try to get your child used to a regular daily toilet routine.
- Do not rush toilet learning. Children can worry and hold back bowel movements if they feel pressured.
- Offer foods that are high in fiber such as whole grain breads, fruits like apples, bananas, berries or prunes, vegetables and legumes (split peas, soy and lentils).
- Give milk and dairy products in amounts that are right for your child’s age.
- After 12 months of age, your child should not take more than 3 portions of milk products per day (one portion of milk = 1 cup or 8 ounces; one portion of yoghurt = ¾ cup or 175 grams; one portion of cheese = 50 grams or 1½ ounces).
- Children between 2 and 8 years need only 2 portions of milk products a day.
- Give your child a firm support for his feet, such as a small stool, when he is passing a bowel movement. It will make it easier to push.
What are symptoms & causes of acute diarrhea?
More bowel movements, with stool that is less formed and more watery than usual.
There are many causes of diarrhea, though it’s usually caused by a virus. The most common cause of acute diarrhea in Canada is a virus called rotavirus. Acute diarrhea usually lasts less than 14 days.
The germs that cause diarrhea, including rotavirus:
- spread easily from person to person, and especially from child to child.
- usually spread easily among children who have not learned to use the toilet.
You can prevent diarrhea caused by rotavirus by having your infant vaccinated. You can also reduce the spread of the virus by washing your hands and your child’s hands carefully after every diaper change, after going to the toilet, and before preparing and eating food.
What can I do if my child has diarrhea?
Children with diarrhea can lose fluids quickly. It’s important to keep offering food and drink to your child.
An oral rehydration solution (ORS), an exact mixture of water, salts and sugar, can be used to help keep your child well hydrated when diarrhea is serious.
What are some causes of chronic diarrhea?
Chronic diarrhea is diarrhea that last for more than 14 days. There are many causes of chronic diarrhea, including disease such as celiac disease (a disease where the body has trouble digesting a protein called gluten).
One fairly common cause of chronic diarrhea in children is often called toddler’s diarrhea.
What is toddler’s diarrhea?
Toddler’s diarrhea usually starts between the ages of 6 and 30 months and will go away by the time your child is about 5 years old. Children with toddler’s diarrhea may have 2 to 6 watery stools each day, but otherwise seem well and gain weight normally.
The exact cause of toddler’s diarrhea isn’t known, but it may be because some food moves more quickly through your child’s colon (the last part of the body’s digestive system).
- Your toddler may drink too many sweetened drinks, such as juice or sports drinks, which can cause loose stool.
- It may also be caused by a lack of fiber in your child’s diet or by eating foods that are too low in fat.
If your toddler has loose, watery stools often:
- Stop offering juice and give water instead. Juice has sugar that can make the diarrhea worse.
- Offer more food with fiber, such as whole grain cereals, fruits and vegetables.
If the diarrhea continues, talk to your doctor at your next regular visit.
Healthy Sleep for Your Baby & Child
Healthy Sleep for Your Baby & Child
How much sleep does my child need?
Sleep is very important to your child’s health and well-being. In fact, good sleep habits start from birth.Children who do not get enough sleep may have trouble getting through the day. At night, they may find it hard to settle.
Every child is different. Some sleep a lot and others much less. This chart is a general guide to the amount of sleep children need over a 24-hour period, including nighttime sleep and daytime naps.
|
Newborns (birth to 2 months) |
16-18 hours a day (3 to 4 hours at a time) |
|
Babies (2 months to 6 months) |
14-16 hours |
|
Older babies (6 months to 1 year) |
14 hours |
|
Toddlers (1 to 3 years) |
10-13 hours |
|
Preschoolers (3 to 5 years) |
10-12 hours |
|
School aged children (5-10 years) |
10-12 hours |
Babies (Birth to 6 months)
Newborns may sleep as much as 16 hours a day, for 3 to 4 hours at a time. It’s normal and healthy for babies to wake up during the night to feed. As your baby gets older, she will stay awake longer during the day and sleep for longer stretches at night.
Babies, just like adults, need the right cues to learn when it is time to sleep. For example, if you always put your baby in her crib to sleep she will learn that this is the place where she sleeps. Even if this doesn’t work right away, over time your baby will come to understand.
Sometime after 3 months, your baby’s sleep habits will become more predictable and you can expect a more regular nap schedule. Trust your baby’s cues – she will let you know when she is tired. A sleep diary might help you to recognize her regular sleeping pattern.
A naptime routine is a good idea. It could include a quiet cuddle and short story in a darkened room before it’s time to nap.
By 4 months, most babies need three naps a day, one in the morning, afternoon and early evening.
Healthy sleep habits for your newborn:
- An overtired baby has more trouble sleeping. Napping actually helps a baby to sleep better at night, so keeping your baby awake during the day will not help your baby sleep longer at night.
- Put your baby in bed when he is drowsy, but awake. Remember to put him to sleep on his back in his crib, on a firm, flat surface. Keep soft items like pillows and stuffed animals out of the crib.
- It’s okay to cuddle and rock your baby. You cannot spoil a newborn baby by holding him.
- A pacifier might be comforting and help your baby to settle. However, it’s best not to start using a pacifier until breastfeeding is going well.
- Your baby will stir during the night. Give him a few minutes to try and settle on his own before going to him.
- Avoid stimulation during nighttime feedings and diaper changes. Keep the lights dim.
Older Babies (6 months to 1 year)
At this age, babies sleep an average of 14 hours in a day, but anything less or more can be normal for your baby. By now you should have a fairly regular routine of naptimes, bedtime and wake times.
During this period your baby will probably change from having 3 naps a day to 2 longer naps, in the morning and afternoon. Every baby’s napping needs are different. Some nap for as little as 20 minutes at a time, while others sleep for 3 or more hours.
Healthy sleep habits for your older baby:
- Maintain a regular daytime and bedtime sleep schedule as much as possible.
- A consistent bedtime routine is important. Many parents like to use the “3 Bs”: bath, book, then settle into bed.
- Don’t put your baby to bed with a bottle. This can lead to tooth decay.
- Babies this age usually don’t need to be fed during night-wakings.
- If your baby wakes at night and cries, go to her to see if there is anything wrong such as being too cold or too warm, but don’t take her out of the crib. Comfort her by stroking her forehead or talking softly to let her know you’re there. This helps your baby learn how to self-soothe, important steps toward falling back to sleep on her own.
Toddlers (1 to 3 years)
Most toddlers sleep between 10 and 13 hours in a 24-hour period. Sometime between 2 and 3 years, your toddler will probably drop to one nap a day, but many will still have a nap at some point in the day. As your child approaches age 3 he can have days when he needs a nap and others when he doesn’t. At this age, it’s common for children to have some sleep problems and to resist going to bed.
Healthy sleep habits for your toddler:
- It’s still important to keep a sleep schedule your child is familiar with. The routine you established during the first year is even more important for your toddler.
- Avoid naps that are too late in the day because they can affect nighttime sleeping.
- Help your child wind down about half an hour before bedtime with stories and quiet activities at around the same time each day.
- Be gentle but firm if your child protests.
- Keep the bedroom quiet, cozy, and good for sleeping, such as keeping the lights dim.
- Soft, soothing music might be comforting.
- Security items (such as a blanket or stuffed animal) are often important at this age.
Preschoolers and young children (4 to 6 years)
Preschoolers typically sleep about 10 to 12 hours a day. Children give up daytime naps during this period. You can use that time—often after lunch—for quiet time for your child to read and relax. At this age, it’s common for children to wake up during the night from nighttime fears or nightmares.
Healthy sleep habits for your preschooler:
- Don’t give your child drinks with caffeine.
- Avoid television before bedtime. Don’t allow television, computer or video games in his bedroom.
- Some children will try to delay bedtime. Set limits, such as how many books you will read together, and be sure your child knows what they are.
- Tuck your child into bed snugly for a feeling of security.
- Don’t ignore bedtime fears. If your child has nightmares, reassure and comfort her.
- What are common sleep problems?
- When should I talk to my doctor?
- What if my child regularly has trouble falling asleep?
- Sleep deprivation: Some children don’t get enough sleep. If your child is fussy, cranky or has difficulty staying asleep at night it might be because he isn’t having enough naptime or isn’t getting to bed early enough.
- Separation issues: Your child may have difficulty relaxing and going to sleep if he feels upset that you are not there. Try an extra long cuddle before bedtime, a security object such as a blanket or stuffed animal, or leaving her door open when you put her to bed.
- Nightmares: Most children will experience nightmares at one time or another. Nightmares can happen after a stressful physical or emotional event or can be caused by fever. Your child may call out to you for comfort. Talk calmly, cuddle and reassure your child.
- Loud snoring: If your child regularly snores loudly, this can be a sign of a problem.
- Sleepwalking: Sleepwalking is a disorder where a child awakens partly, but not completely, during the night. Your child may sit up in bed and repeat certain movements, such as rubbing her eyes. She may get out of bed and walk around the room. When you talk to your child, she usually won’t answer you. If your child sleepwalks it is important that you ensure the area is safe. Gently guide your child back to bed without waking her. If the problem continues, contact your doctor.
- Night terrors: These are different from nightmares. Children with night terrors scream uncontrollably, may breathe quickly, and seem to be awake. If you wake your child, he’s likely to be confused, and may take longer to settle down and go back to sleep. They usually happen between the ages of 4 and 12, but can happen to children as young as 18 months. Most children will outgrow them, but if they persist talk to your doctor.
Some children have trouble falling to sleep on their own and can lay awake for long periods of time. This can be caused by too much screen time before bed, or caffeine from soda and energy drinks.
- If your child is watching TV or playing video games for long periods of time, try limiting screen time or cutting it out of her routine.
- Don’t allow your child to drink or eat anything with caffeine.
- Try doing relaxing activities before bed such as reading, listening to calming music, or laying in bed with your child talking quietly about her day.
If these reasons aren’t the cause, talk to your doctor about other ways to help your child learn to fall asleep on her own.
Jaundice in Newborns
Jaundice in Newborns
What is jaundice?
Jaundice is very common in newborn babies. It makes a baby’s skin and the whites of the eyes turn a yellow color. Most jaundice is not severe and complications can usually be prevented.
Jaundice is a condition where a newborn baby’s skin turns yellow because a high amount of bilirubin is produced or because the liver can’t get rid of it quickly enough. Bilirubin is a brownish-yellow substance that is produced after red blood cells have been broken down. The body gets rid of bilirubin through the stool (poo).
How is jaundice treated?
Most of the time, jaundice goes away on its own. Sometimes babies will need help to get their bilirubin levels down. One way to do this is with phototherapy, where your baby’s skin is exposed to light. The skin absorbs the light and changes the bilirubin so that his body can more easily get rid of it in stool and urine. Phototherapy is usually done in a hospital, but sometimes babies can be treated at home. Exposing your baby to sunlight (directly or indirectly) can be harmful. Do not do this without first discussing with your health care provider.
Is Phototherapy safe?
Phototherapy is safe. Your baby’s eyes will be protected with special eye patches. Phototherapy can sometimes cause skin rash or loose bowel movements. Your baby may need extra fluids, such as more frequent breastfeeding.
When should I be more concerned about jaundice?
Jaundice can be more serious for some babies, including babies:
- born before 37 weeks gestation.
- who weigh less than 2500 grams (5.5 lbs) at birth.
- whose blood group is incompatible with their mothers’ blood group.
- who develop jaundice early in life, especially during the first 24 hours.
- whose jaundice has moved into the arms and legs.
- who have a lot of bruising or swelling under the scalp (called caput) after birth
- whose siblings had jaundice at birth and needed treatment with an exchange transfusion (baby’s blood is removed and replaced).
What are the symptoms of jaundice?
Jaundice is very common in newborn babies. It makes a baby’s skin and the whites of the eyes turn a yellow color. You may notice it between 1 and 4 days after your baby is born. It will first appear on your baby’s face and chest.
Babies who have higher levels of bilirubin (severe jaundice) may seem very tired and cranky, and feed poorly because they are too hard to wake up.
Will jaundice hurt my baby?
Most jaundice is not harmful to your baby and disappears when your baby’s body learns to deal with bilirubin. But in some babies there is so much bilirubin that it can be harmful. If the level of bilirubin becomes very high it can affect some of your baby’s brain cells.
In rare cases, severe jaundice can cause seizures (convulsions) or lead to deafness, cerebral palsy or serious developmental delay. Fortunately, most jaundice is not severe and complications can usually be prevented.
How can I prevent jaundice?
Feeding (especially breastfeeding) your baby frequently in the first hours and days after his birth helps reduce the risk of jaundice. Feeding often will make your baby pass more stool. The milk also gives your baby’s liver the energy it needs to process the bilirubin. Your baby’s stool should turn from dark green to yellow.
If you are having trouble with breastfeeding, it is important to get help. It might be necessary to offer your baby supplementary feeds of formula to avoid dehydration and to keep the jaundice from getting worse.
How do I know if my baby’s bilirubin levels are too high?
There is a blood test to measure the amount of bilirubin in your baby’s body. In many hospitals, bilirubin levels are routinely checked before you take your baby home. Your health care provider can plot your baby’s result on a graph if they know exactly how many hours old your baby was when the test was performed.
The information should be given to you when you and your baby leave the hospital. If the test shows that your baby is at risk for reaching a level of bilirubin that needs treatment, your doctor will arrange a follow-up visit and will do another test.
After I leave the hospital, when should I call my doctor?
Call your doctor if your baby shows any of the following symptoms:
- refuses breastfeeding or bottle feeding,
- is sleepy all the time,
- has lost a lot of weight (more than 10% of her weight at birth),
- is extremely jaundiced (arms and legs are a yellow or orange color), or
- jaundice that seems to be getting worse.





Recent Comments