Weaning Your Child From Breastfeeding
Weaning Your Child From Breastfeeding
Weaning is a natural stage in your baby’s development. It is the gradual process of giving your baby other foods while continuing to breastfeed.
- Breastfeeding as long as you can is the best thing for your baby.
- As you introduce your baby to new foods, you can continue to breastfeed.
- It’s easiest for you and your baby if weaning is gradual.
- The right complementary food will depend on your baby’s age when you start to wean.
Weaning can come with a lot of mixed emotions. You may feel excited at the new independence you and your baby can both enjoy, as well as some sadness as your baby moves to another stage in her life. This is completely normal.
Breastfeeding as long as you can is the best thing for your baby. You can continue to breastfeed until your child is 2 years of age and beyond.
At about 6 months, your baby will be ready for other foods. He will also need other foods to meet his growing nutritional needs. As you introduce your baby to new foods, you can continue to breastfeed.
You’ll know baby is ready to start other foods when he:
- Seems hungry earlier than usual.
- Can sit up without support, and has good control of his neck muscles.
- Holds food in his mouth without pushing it out on his tongue right away.
- Shows interest in food when others are eating.
- Opens his mouth when he sees food coming his way.
- Can let you know he doesn’t want food by leaning back or turning his head away.
Weaning can be either natural (child-led) or planned (mother-led). Natural weaning or “child-led weaning” happens when your baby starts to accept more—and different types—of solid foods while still breastfeeding on demand. With this type of weaning, you watch your baby’s cues and wean at her pace. Babies who are weaned naturally usually stop breastfeeding completely sometime between 2 and 4 years of age.
Planned weaning or “mother-led weaning” happens when mothers decide to start the weaning process. A “partial wean” means substituting one or more feedings with a cup or bottle and breastfeeding at other times. This can work well if you are going back to work or school, but still want to breastfeed. Early morning, evening and night feedings can continue even if you are separated from your baby during the day.
Your weaning experience is up to you and your baby. Try to follow your baby’s cues whenever possible. If you feel your baby is not taking what you think is enough other foods or liquids, see your doctor.
When you and your baby are ready to wean, there are few things that can help make the experience a more positive one for both of you:
- It’s easiest for you and your baby if weaning is gradual – over several weeks, months or even longer. A sudden, abrupt wean should only be considered in extreme circumstances such as maternal illness.
- Start by substituting one feed. When one feed is going well, substitute another feed, and so on.
- Continue this way, substituting one feed at a time. The pace is up to you and your baby, but in general, the slower the better.
- Someone else, such as your baby’s father, may need to offer a feed for your baby to accept it. You can start with a liquid (such as expressed breast milk) in a bottle or cup or a complementary food after about 6 months of age.
- Follow your baby’s cues. She’ll tell you when she’s had enough.
- Hold and cuddle your baby if you are feeding from a bottle. This extra closeness will help both of you during the weaning process. Never prop a bottle. Bottle propping can put your baby at risk for choking and causes early childhood caries.
Watch the cues you give to your baby. If you sit in the same chair you usually use when you’re nursing, he’ll likely want to breastfeed
If possible, avoid an abrupt wean, which can be uncomfortable for you and upsetting for your baby.
- If you have to take a medication, talk to your doctor. There are very few medications that require you have to stop breastfeeding.
- If you are very sick, or if you and your baby have to be separated or a long time, try some of the suggestions for caring for your breasts described below. If your breasts get uncomfortable, express your milk to avoid blocked ducts, mastitis or a breast abscess.
- Babies who are sick should NOT be abruptly weaned. You can pump and store breast milk until your baby can take it again.
What complementary foods can I give my baby?
At about 6 months, you’ll start to introduce solid foods into your baby’s diet. When this happens, your baby will begin to take less breast milk.
Introduce solids one at a time and in small amounts at the beginning. Some babies get very constipated if they are given too much solid food early on.
You can also offer your baby small amounts of water once or twice a day, usually after 6 months of age. It’s best not to offer juice at this age. Too much juice can lead to dental caries, obesity or even poor weight gain and diarrhea.
If you give your baby water, or alternate milks, offer it in a cup instead of a bottle. Breastfed babies easily learn to drink from a cup as early as 6 months of age. You can also try this with expressed breast milk.
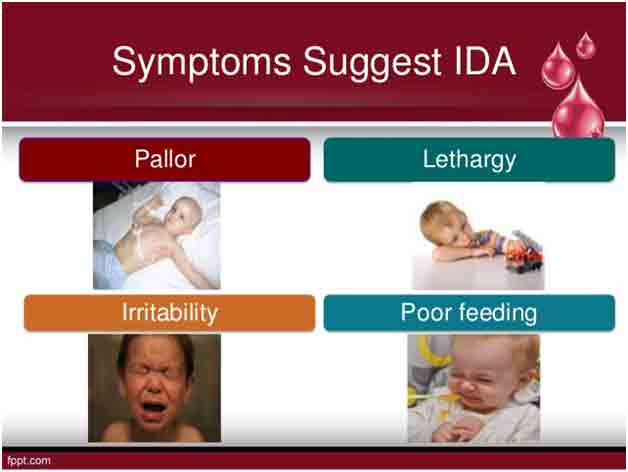
After 12 months of age, your baby should not take more than 16 to 24 ounces (500 mL to 720 mL) of milk per day. Otherwise, she’ll fill up and won’t want to eat solid foods. Also, she may develop iron deficiency anemia. If your baby has a milk allergy, talk to your doctor about what to use for substitute feedings.
| Age | What to offer |
| 6 to 12 months |
|
| 12 to 18 months |
|
| 18 to 24 months |
|
| 2 to 5 years |
|
My baby is refusing the breast. Does that mean he’s ready to wean?
No, it doesn’t necessarily mean your baby is ready to wean. Sometimes babies go on a “nursing strike” and suddenly refuse to breastfeed. There can be many causes, such as teething, an ear infection or other illness, the onset of your period, a change in your diet, soap, or even deodorant.
Here are some tips to encourage your baby to start breastfeeding again:
- Make feeding time special and quiet; try to limit distractions. Sometimes, as babies get older, they are more interested in looking at the things happening around them then focusing on nursing.
- Cuddle and soothe your baby as much as possible.
- Offer your breast when your baby is very sleepy or just waking up.
- If possible, try using different nursing positions, alternate sides, or nurse in different rooms.
- If you can’t figure out the reason for your baby’s nursing strike, see your doctor or talk to a lactation consultant. Don’t get frustrated or angry. Remember that a nursing strike does not mean your baby is rejecting you.
If this happens, be sure to pump your milk so you don’t develop a blocked duct and that you continue to produce enough breast milk for when your baby is ready to nurse again.
Should I care for my breasts when I start to wean?
- If your breasts are uncomfortable while weaning, try expressing some milk. Over-the-counter pain relievers like acetaminophen or ibuprofen might help. Cold compresses or gel packs applied to your breasts can also be of some comfort.
- Don’t bind your breasts or drink fewer fluids while you’re weaning.
- Check your breasts regularly to make sure you aren’t developing a blocked duct. A block duct will feel like a firm, tender area (the size of a pea) of the breast. Sometimes you can clear it with gentle rubbing or by putting a little bit of pressure on the area. If it’s painful, see your doctor or lactation consultant. This is more likely to occur during an abrupt wean.
What is mastitis?
Mastitis is an infection that causes breast pain, swelling, warmth and redness on your breast. It can also cause fever and chills. If you have these symptoms, call your doctor. Your doctor will most likely prescribe an antibiotic to clear up the infection. You can continue breastfeeding if you have mastitis.
Where can I get more information?
You probably have many questions about breastfeeding and your baby’s nutrition. There are many sources of information, including your paediatrician, family doctor, a community health nurse, breastfeeding clinic, and lactation consultant.





Recent Comments